Parenteral nutrition delivers nutrients directly into the bloodstream through intravenous methods, bypassing the digestive system entirely. Enteral nutrition involves feeding through the gastrointestinal tract using methods like oral intake, feeding tubes, or gastrostomy, supporting digestive function. Explore the key differences and applications of parenteral versus enteral nutrition to optimize patient care strategies.
Main Difference
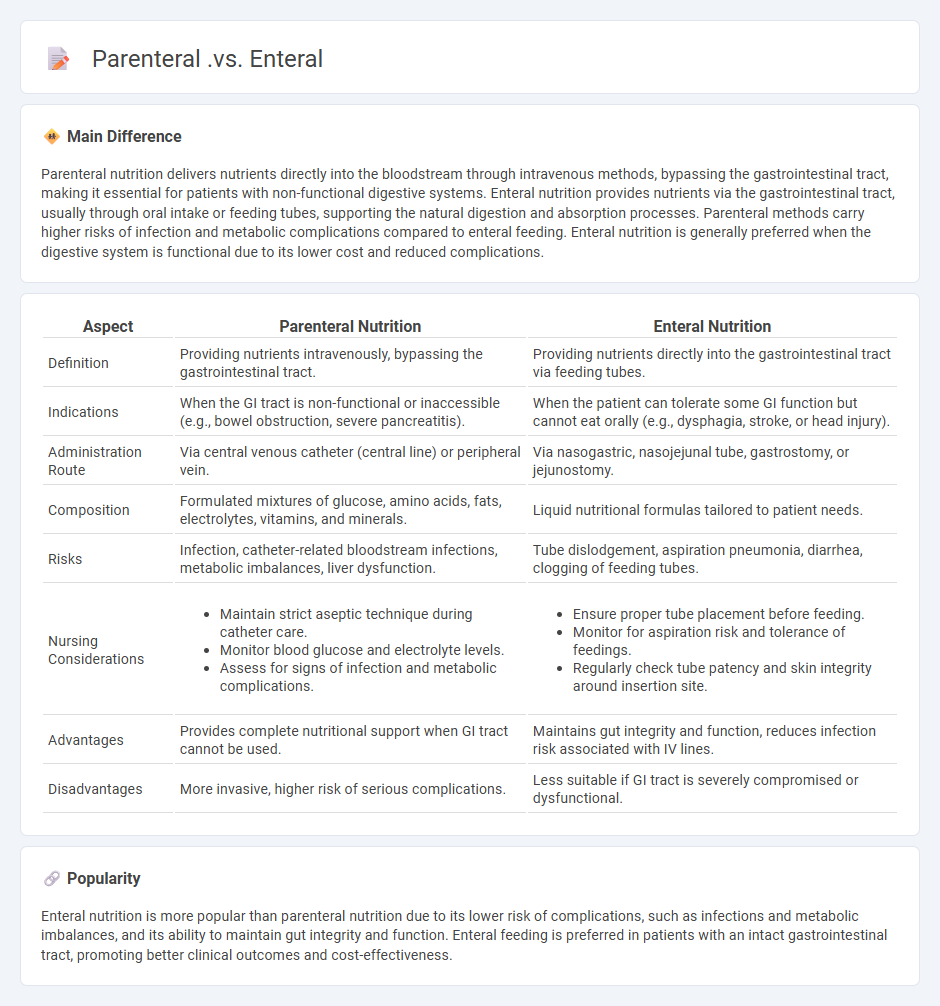
Parenteral nutrition delivers nutrients directly into the bloodstream through intravenous methods, bypassing the gastrointestinal tract, making it essential for patients with non-functional digestive systems. Enteral nutrition provides nutrients via the gastrointestinal tract, usually through oral intake or feeding tubes, supporting the natural digestion and absorption processes. Parenteral methods carry higher risks of infection and metabolic complications compared to enteral feeding. Enteral nutrition is generally preferred when the digestive system is functional due to its lower cost and reduced complications.
Connection
Parenteral and enteral nutrition are interconnected methods of providing essential nutrients to patients unable to consume food orally. Enteral nutrition delivers nutrients directly to the gastrointestinal tract through feeding tubes, while parenteral nutrition bypasses the digestive system by administering nutrients intravenously. Both techniques are critical in medical settings to ensure adequate nutritional support tailored to a patient's clinical condition.
Comparison Table
| Aspect | Parenteral Nutrition | Enteral Nutrition |
|---|---|---|
| Definition | Providing nutrients intravenously, bypassing the gastrointestinal tract. | Providing nutrients directly into the gastrointestinal tract via feeding tubes. |
| Indications | When the GI tract is non-functional or inaccessible (e.g., bowel obstruction, severe pancreatitis). | When the patient can tolerate some GI function but cannot eat orally (e.g., dysphagia, stroke, or head injury). |
| Administration Route | Via central venous catheter (central line) or peripheral vein. | Via nasogastric, nasojejunal tube, gastrostomy, or jejunostomy. |
| Composition | Formulated mixtures of glucose, amino acids, fats, electrolytes, vitamins, and minerals. | Liquid nutritional formulas tailored to patient needs. |
| Risks | Infection, catheter-related bloodstream infections, metabolic imbalances, liver dysfunction. | Tube dislodgement, aspiration pneumonia, diarrhea, clogging of feeding tubes. |
| Nursing Considerations |
|
|
| Advantages | Provides complete nutritional support when GI tract cannot be used. | Maintains gut integrity and function, reduces infection risk associated with IV lines. |
| Disadvantages | More invasive, higher risk of serious complications. | Less suitable if GI tract is severely compromised or dysfunctional. |
Route of Administration
The route of administration in nursing refers to the specific path by which a medication or substance is delivered into the body, including oral, intravenous, intramuscular, subcutaneous, and topical methods. Each route affects the drug's absorption rate, bioavailability, onset of action, and patient compliance, necessitating careful selection based on clinical indications and patient condition. Intravenous administration provides immediate systemic effects, while oral routes are non-invasive but subject to first-pass metabolism in the liver. Proper technique and understanding of pharmacokinetics ensure safe and effective medication delivery in nursing practice.
Absorption Process
The absorption process in nursing refers to the movement of nutrients, medications, or substances from the site of administration into the bloodstream. This process varies based on the route of administration, such as oral, intravenous, or intramuscular, influencing the onset and intensity of therapeutic effects. Factors like blood flow, solubility, and pH at the absorption site critically impact the bioavailability of medications administered to patients. Understanding absorption kinetics is essential for nurses to optimize drug efficacy and patient outcomes.
Indications and Contraindications
Nursing protocols include specific indications for administering medications, performing procedures, and providing patient care based on clinical assessments and diagnostic criteria. Common indications involve managing symptoms, preventing complications, and improving patient outcomes in conditions such as infections, chronic diseases, and postoperative recovery. Contraindications highlight situations where certain interventions may cause harm, including allergies, contraindicated medication interactions, and unstable patient vital signs. Understanding these parameters ensures nurses deliver safe, effective, and evidence-based care aligned with health standards.
Complications and Risks
Complications and risks in nursing include healthcare-associated infections (HAIs), medication errors, and patient falls, which significantly impact patient safety and outcomes. Pressure ulcers affect approximately 2.5 million hospitalized patients annually in the United States, emphasizing the importance of early risk assessment and preventive measures. Medication administration errors occur in about 5-10% of doses, highlighting the need for strict adherence to protocols and double-check systems. Effective communication, continuous staff education, and adherence to evidence-based practices are critical in minimizing these complications and improving overall patient care quality.
Nutritional Formulations
Nutritional formulations in nursing play a crucial role in patient recovery by providing tailored macronutrient and micronutrient support. These formulations include enteral nutrition options such as polymeric, oligomeric, and elemental formulas, designed to meet specific dietary needs according to clinical conditions like malnutrition, gastrointestinal disorders, or critical illness. Precise assessment of caloric requirements, protein intake, and fluid balance is essential for optimizing the effectiveness of nutritional interventions. Evidence-based protocols ensure improved clinical outcomes, reduce complication rates, and support overall patient health during hospital stays.
Source and External Links
Enteral vs. Parenteral Feeding & Nutrition: A Complete Guide - Enteral feeding delivers nutrition directly to the gastrointestinal tract via a feeding tube, using the body's natural digestion, while parenteral feeding bypasses the GI tract, delivering nutrients intravenously through a vein, often used when the GI tract is nonfunctional or inaccessible.
Enteral and Parenteral Nutrition - Enteral nutrition involves feeding through the GI tract (oral, tube feeding), preferred when possible due to its use of natural digestive pathways, whereas parenteral nutrition delivers nutrients directly into the bloodstream intravenously, used when enteral feeding is unsafe or insufficient.
Enteral and Parenteral Nutrition - Enteral nutrition is generally preferred for being more physiological, simpler, cheaper, and less complicated; parenteral nutrition is reserved for cases where the gut cannot absorb nutrients due to obstruction, perforation, or disease and involves intravenous delivery with higher risk and need for monitoring.
FAQs
What does parenteral mean?
Parenteral means administering substances, especially medications or nutrition, by injection through routes other than the digestive tract, such as intravenous, intramuscular, or subcutaneous methods.
What does enteral mean?
Enteral refers to anything related to or occurring within the intestines, often used to describe nutrient administration through the digestive tract.
How are parenteral and enteral nutrition different?
Parenteral nutrition involves delivering nutrients intravenously, bypassing the gastrointestinal tract, whereas enteral nutrition provides nutrients directly into the stomach or intestines through a feeding tube.
When is parenteral nutrition used?
Parenteral nutrition is used when a patient cannot obtain adequate nutrients through oral or enteral feeding due to conditions like severe gastrointestinal disorders, bowel obstruction, short bowel syndrome, or during critical illness.
What are the risks of parenteral nutrition?
Risks of parenteral nutrition include infections, metabolic complications like hyperglycemia and electrolyte imbalances, liver dysfunction, catheter-related bloodstream infections, and nutrient deficiencies or toxicities.
Which conditions require enteral feeding?
Conditions requiring enteral feeding include dysphagia, neurological disorders (e.g., stroke, Parkinson's disease), head and neck cancers, critical illness impairing oral intake, severe malnutrition, and gastrointestinal dysfunction where the gut is functional but oral intake is insufficient.
What are the benefits of enteral over parenteral nutrition?
Enteral nutrition preserves gut integrity, reduces infection risk, lowers healthcare costs, and enhances immune function compared to parenteral nutrition.
 calledges.com
calledges.com