Euthymia refers to a normal, stable mood state characterized by feelings of well-being and contentment, whereas dysthymia is a chronic form of mild depression marked by persistent low mood and diminished interest in activities. The Diagnostic and Statistical Manual of Mental Disorders (DSM-5) classifies dysthymia as Persistent Depressive Disorder, requiring symptoms lasting for at least two years. Explore further to understand the clinical distinctions and treatment approaches for these mood conditions.
Main Difference
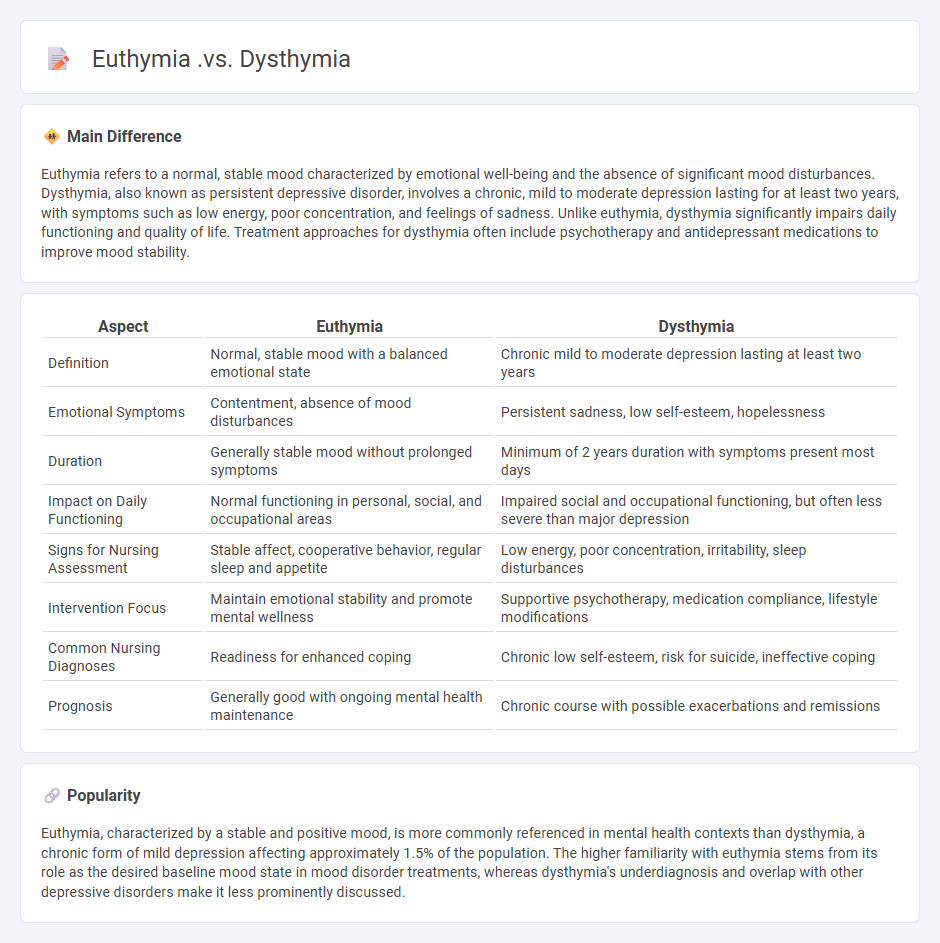
Euthymia refers to a normal, stable mood characterized by emotional well-being and the absence of significant mood disturbances. Dysthymia, also known as persistent depressive disorder, involves a chronic, mild to moderate depression lasting for at least two years, with symptoms such as low energy, poor concentration, and feelings of sadness. Unlike euthymia, dysthymia significantly impairs daily functioning and quality of life. Treatment approaches for dysthymia often include psychotherapy and antidepressant medications to improve mood stability.
Connection
Euthymia represents a stable, normal mood state often associated with psychological well-being, while dysthymia is characterized by chronic, mild to moderate depressive symptoms lasting for at least two years. The connection lies in their positioning on the mood spectrum, with euthymia serving as the baseline mood state from which dysthymia deviates due to persistent low mood and functional impairment. Understanding this relationship aids in differentiating between normal mood variations and clinically significant depressive disorders for accurate diagnosis and treatment.
Comparison Table
| Aspect | Euthymia | Dysthymia |
|---|---|---|
| Definition | Normal, stable mood with a balanced emotional state | Chronic mild to moderate depression lasting at least two years |
| Emotional Symptoms | Contentment, absence of mood disturbances | Persistent sadness, low self-esteem, hopelessness |
| Duration | Generally stable mood without prolonged symptoms | Minimum of 2 years duration with symptoms present most days |
| Impact on Daily Functioning | Normal functioning in personal, social, and occupational areas | Impaired social and occupational functioning, but often less severe than major depression |
| Signs for Nursing Assessment | Stable affect, cooperative behavior, regular sleep and appetite | Low energy, poor concentration, irritability, sleep disturbances |
| Intervention Focus | Maintain emotional stability and promote mental wellness | Supportive psychotherapy, medication compliance, lifestyle modifications |
| Common Nursing Diagnoses | Readiness for enhanced coping | Chronic low self-esteem, risk for suicide, ineffective coping |
| Prognosis | Generally good with ongoing mental health maintenance | Chronic course with possible exacerbations and remissions |
Mood Stability
Mood stability in nursing is crucial for maintaining optimal mental health and ensuring effective patient care. Nurses experiencing mood stability demonstrate consistent emotional regulation, which enhances decision-making, communication, and stress management during demanding healthcare situations. Research shows that stable mood correlates with reduced burnout rates and improved job satisfaction among nursing professionals. Implementing mindfulness strategies, cognitive-behavioral interventions, and supportive workplace environments significantly supports mood stability in nursing staff.
Persistent Depressive Disorder
Persistent Depressive Disorder (PDD), also known as dysthymia, is a chronic form of depression characterized by a depressed mood lasting for at least two years. Nursing care for patients with PDD involves continuous monitoring of mood, medication adherence, and promoting therapeutic communication to address emotional needs. Interventions focus on improving daily functioning through cognitive-behavioral strategies and fostering social support networks. Understanding the prolonged course of PDD helps nurses tailor individualized care plans that reduce symptom severity and enhance quality of life.
Emotional Baseline
Emotional baseline in nursing refers to a nurse's typical emotional state during patient care, influencing empathy, communication, and decision-making. Maintaining a stable emotional baseline is essential for reducing burnout, enhancing patient outcomes, and improving professional resilience. Research shows that mindfulness and stress management techniques help nurses sustain an optimal emotional baseline amid high-pressure healthcare environments. Healthcare organizations often incorporate emotional baseline assessments in training to support nurse well-being and quality patient interactions.
Symptom Duration
Symptom duration in nursing is a critical factor for assessing patient conditions and planning appropriate care interventions. Accurate documentation of the length of time symptoms have been present aids in differential diagnosis and evaluating the progression or resolution of illnesses. Nurses use standardized tools like the symptom checklist and electronic health records (EHR) to track symptom duration consistently. Monitoring these timeframes contributes to improved patient outcomes and informs evidence-based practice guidelines in clinical settings.
Treatment Strategies
Effective treatment strategies in nursing emphasize patient-centered care plans tailored to individual health conditions and needs. Evidence-based interventions, such as medication management, wound care, and patient education, form the foundation of nursing treatments. Incorporating multidisciplinary collaboration improves outcomes by addressing complex health issues comprehensively. Utilizing technology like electronic health records enhances accuracy and continuity of care in nursing practice.
Source and External Links
Cyclothymia vs. Dysthymia: What's the Difference? - Dysthymia (persistent depressive disorder) is a chronic low mood lasting at least two years with symptoms like fatigue and low self-esteem, while euthymia refers to a normal, stable mood without mood disturbances.
Dysthymia - Dysthymia, now called persistent depressive disorder, is characterized by a chronic depressed mood lasting two years or more, with symptoms similar to major depression but less severe and more enduring.
Euthymia: a neglected aspect of trait depression and its ... - Euthymia is conceptualized as the presence of positive emotional experiences and well-being (depression-absence factor), contrasting with dysthymia, which involves negative emotional experiences (depression-presence factor).
FAQs
What is euthymia?
Euthymia is a stable mental state characterized by normal mood, absence of depression or mania, commonly used to describe balanced mood in bipolar disorder.
What is dysthymia?
Dysthymia, also known as persistent depressive disorder, is a chronic form of depression characterized by a depressed mood lasting for at least two years in adults, accompanied by symptoms such as low energy, low self-esteem, and feelings of hopelessness.
How does euthymia differ from dysthymia?
Euthymia is a normal, stable mood state characterized by emotional well-being, while dysthymia, or persistent depressive disorder, is a chronic form of mild depression lasting at least two years with symptoms like low mood, fatigue, and low self-esteem.
What are the main symptoms of dysthymia?
The main symptoms of dysthymia include persistent low mood, low energy, poor appetite or overeating, sleep disturbances, low self-esteem, difficulty concentrating, and feelings of hopelessness lasting for at least two years.
Can someone with dysthymia experience euthymia?
Individuals with dysthymia can experience periods of euthymia, characterized by stable, normal mood between depressive episodes.
How is euthymia maintained in mental health?
Euthymia in mental health is maintained through consistent medication adherence, regular psychotherapy, balanced lifestyle habits, stress management techniques, and ongoing psychiatric evaluation.
What treatments help manage dysthymia?
Cognitive-behavioral therapy (CBT), antidepressant medications such as selective serotonin reuptake inhibitors (SSRIs), lifestyle changes including regular exercise, and psychotherapy effectively manage dysthymia.
 calledges.com
calledges.com